What is Dacryocystitis in Children?
Dacryocystitis in children is an inflammation of the lacrimal sac. It occurs in 2-7% of patients with diseases of the lacrimal organs. Female children are affected by the disease 6-10 times more often than male children.
Classification
Forms of the course of dacryocystitis:
- acute
- chronic
Forms of chronic dacryocystitis:
- simple
- ectatic catarrhal
- stenosing
- empyema of the lacrimal sac
- phlegmon of the lacrimal sac.
Separately, in the literature, dacryocystitis of newborns is considered, which can take the following forms:
- simple
- ectatic catarrhal
- purulent
- phlegmonous.
Acute dacryocystitis in most cases occurs as a result of a chronic process (but – rarely – it can also be an independent form of the disease). This is a purulent inflammation of the walls of the lacrimal sac. If the surrounding tissue is further involved in the process, phlegmon of the lacrimal sac appears.
Types of dacryocystitis by etiology:
- viral,
- bacterial,
- parasitic,
- chlamydial,
- post-traumatic.
Causes of Dacryocystitis in Children
Stenosis of the nasolacrimal canal and stagnation of tears in the lacrimal sac leads to dacryocystitis in children. The lacrimal sac is located in the fossa of the lacrimal sac at the medial angle of the orbit – the lacrimal tubules flow into it.
Dacryocystitis in newborns is most often caused by atresia of the outlet of the nasolacrimal duct.
Pathogenesis during Dacryocystitis in Children
The outflow of tears is disrupted, and this leads to the development of pathogenic flora in the lacrimal sac. By pathogenic flora is meant pathogenic microorganisms, which, entering the human body (including its mucous membranes), cause various diseases and dysfunctions.
The outflow of tears is difficult due to inflammation of the mucous membrane of the nasolacrimal duct, which in most cases passes from the nasal mucosa.
Symptoms of Dacryocystitis in Children
Symptoms of acute dacryocystitis:
- lacrimation
- redness and swelling in the inner corner of the palpebral fissure
- sharp pain in the inner corner of the palpebral fissure.
On examination, doctors detect swelling and hyperemia of tissues in the area of the lacrimal sac, adjacent areas of the nose and cheeks. These tissues are dense on palpation, painful sensations arise. If the edema is pronounced, the palpebral fissure narrows. In the first days of the disease, pus is released from the lacrimal openings if you lightly press on the area of the lacrimal sac.
At first, the tubular test shows a positive result, later the tubular and nasal tests become negative. The child has the following symptoms:
- weakness
- high temperature
- headache.
A few days later, the softening of the infiltrate is recorded, and fluctuation appears. Fluctuation is understood as the presence of fluid in the cavity (pus, blood, etc.). An abscess appears, which can be opened for no apparent reason and without surgery.
In newborns with dacryocystitis, mucus and pus are secreted from the lacrimal openings. Tubular test positive, nasal test negative. When the lacrimal passages are flushed, the liquid does not pass into the nasal cavity. There may be a complication of the type of phlegmonous acute dacryocystitis.
Diagnosis of Dacryocystitis in Children
Diagnosis requires a typical clinical picture, complaints characteristic of dacryocystitis, external examination, palpation of the lacrimal sac region. Doctors, upon examination, reveal the symptoms described above.
It is necessary to conduct a study of the patency of the lacrimal passages. To do this, put a color test Vesta, known more as a tubular test. The procedure consists in inserting a tampon into the nasal passage, and a collargol solution is instilled into the eye. If the lacrimal passages are patent, dye is visible on the tampon for two minutes. If the tampon is stained in 5-10 minutes, the patency of the lacrimal passages is impaired. If in 10 minutes traces of the dye are not visible on the tampon, Vest’s test is negative, which indicates that there is no patency in the lacrimal ducts.
To clarify the extent and level of the lesion, diagnostic probing of the lacrimal canals is performed. Confirmation of obstruction of the lacrimal ducts with dacryocystitis in children can be done using a passive nasolacrimal test. The procedure consists in the fact that the liquid does not pass into the nose when the lacrimal-nasal canal is flushed – it flows out in a stream through the lacrimal openings.
When diagnosing dacryocystitis, biomicroscopy of the eye and a fluorescein instillation test are also used. To have an idea of the structure of the lacrimal duct, contrast radiography of the lacrimal duct is made with iodolipol solution. The localization of the zone of stricture or obliteration is clarified in the same way.
To clarify the microbial pathogens of the disease, a study should be carried out from the lacrimal openings – bacteriological inoculation is used. If the diagnosis is complicated, the child can be examined by an otolaryngologist and a rhinoscopy performed. Also, a traumatologist, maxillofacial surgeon, neurosurgeon, neurologist can be involved in the diagnosis. Dacryocystitis is distinguished in diagnosis from conjunctivitis, erysipelas and canaliculitis.
Treatment of Dacryocystitis in Children
Acute dacryocystitis in children is treated in a hospital. As long as no fluctuation symptoms are observed, UHF therapy and dry heat can be used. Taking multivitamins is required.
When fluctuation appears, the phlegmon must be opened. After that, drainage is carried out with a 10% sodium chloride solution. For 3 to 7 days, the wound should be washed with antiseptic solutions (for example, dioxidine solution). The wound will gradually cleanse, this area needs to be lubricated for 5-7 days three to four times a day with agents that improve the healing process, for example, 5-10% methyluracil ointment. Magnetotherapy is used in parallel with the described procedures.
For 1 week to 10 days, antimicrobial solutions are instilled into the conjunctival sac:
- sodium sulfacyl solution 10-20%,
- Miramistin solution 0.01%,
- gentamicin solution 0.3%,
- solution of chloramphenicol 0.25%,
- Colbiocin,
- Tsipromed,
- Oriprim-P or Trimethoprim.
In the same course (7-10 days), antibacterial ointments, for example, erythromycin, tetracycline, etc., should be placed in the conjunctival sac before bedtime.
Orally or parenterally, a course of 7 to 10 days, broad-spectrum antibiotics or sulfa drugs are taken. The maximum effect is provided by bacteriostatic (sulfanilamide) and bactericidal drugs in combination.
Antibiotics for the treatment of dacryocystitis in children:
- Penicillins with a course of 5 to 14 days – have a bactericidal effect. Inside take ampicillin, oxacillin. Ampicillin, oxacillin, benzylpenicillin sodium salt is injected intramuscularly (it is also administered intravenously).
- Aminoglycosides with a course of 5 to 10 days – have a bactericidal effect, like penicillins. They are administered intravenously or intramuscularly. Gentamicin is used twice a day.
- Cephalosporins with a course of 5 to 14 days – have a bactericidal effect. They are administered intravenously or intramuscularly. The effect is provided by ceftriaxone and cefotaxime.
- Sulfanilamide drugs with a course of 5 to 14 days – have a bacteriostatic effect. Inside take sulfadimidine, co-trimoxazole.
If the symptoms of intoxication are pronounced, the doctor may prescribe an intravenous drip for 1 to 3 days of hemodez solution, 200-400 ml each, 5% glucose solution, 200-400 ml each with ascorbic acid 2 g.
For 5 to 10 days, intravenous administration of 10% calcium chloride solution, 10 ml each, and 10 ml hexamethylenetetramine solution (Urotropin) should be alternated.
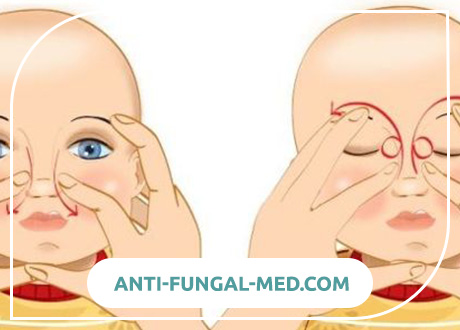
Treatment of dacryocystitis in newborns is carried out, starting with a jerky massage from top to bottom of the lacrimal sac. It needs to be carried out 3 to 4 times a day for a course of 10-15 days.
After the massage, antiseptic solutions are instilled into the baby’s conjunctival sac:
- Miramistin solution 0.01%
- Picloxidine solution 0.05%
- Furatsilin solution 1: 5000.
If the positive effect does not occur in 1-2 weeks, passive lavage of the lacrimal passages with a solution of furacilin 1: 5000 should be performed. If after massage and rinsing, recovery does not come, doctors prescribe sounding with a Bowman probe.
Evaluation of the effectiveness of treatment
After the symptoms of acute dacryocystitis “have subsided”, tearing can still last for a long time. Timely surgical treatment is needed to help restore tear drainage.
Prevention of Dacryocystitis in Children
Diseases of the ENT organs (ear, throat, nose) should be adequately and timely treated, and injuries to the eyes and facial skeleton should be avoided. If you find one or more of the above symptoms in yourself, consult a doctor, because such symptoms can also appear in other diseases of the ENT organs.